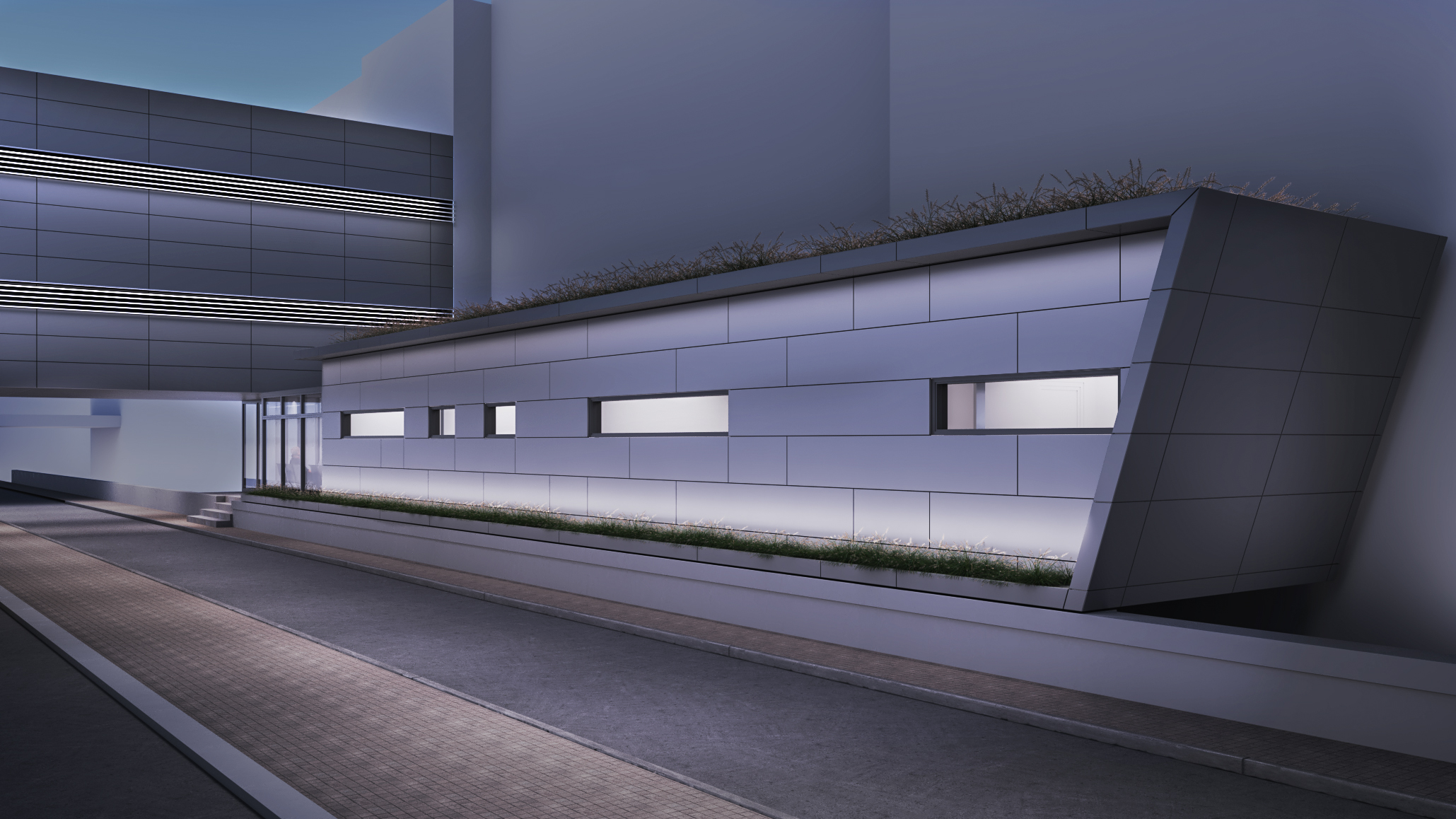
Running a More Efficient Emergency Department and Remodeling ICU.
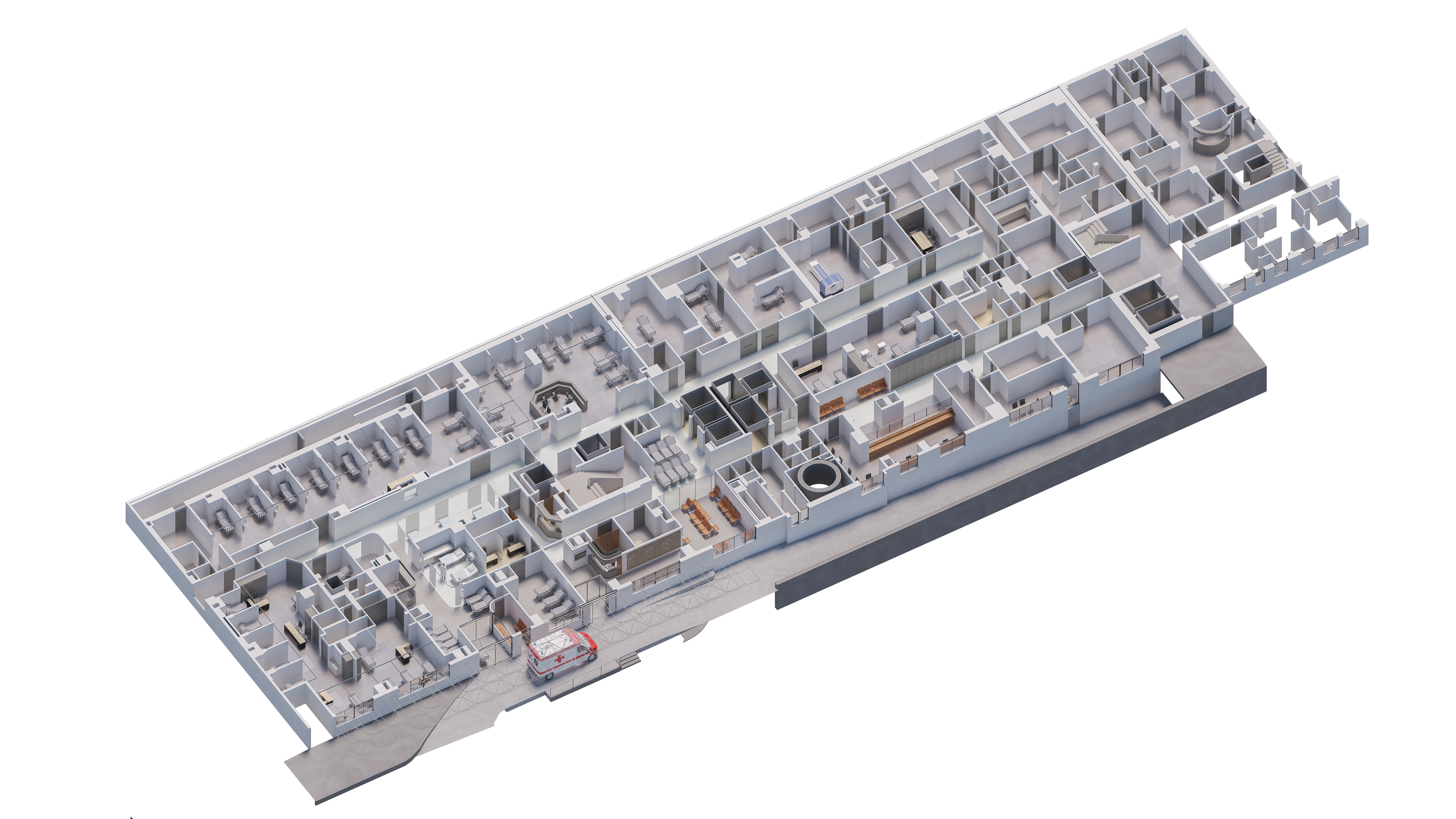
The goal in renovating the emergency department at Evangelismos Athens General Hospital was to streamline patient intake, registration and the triage process. Using a “split flow” operational model allows higher acuity patients to be seen immediately and reduces the wait time for patients with less acute conditions. The layout allows the space for clinical operations to flex up or down based on patient volume.
Forward-looking design enables hospital to adapt to changing needs, such as technology enhancements and continuing patient volume increases in the future.
Emergency departments (ED) operate as the gateway to a hospital.
Flow through the ED can be thought of as an elaborate system of interconnected queues, comprising three major consecutive queue processes:
- The Door to Doctor Interval, including Door to Triage and Triage to Bed Assignment
Reduce time from patient arrival to physician consult. This is the most important interval from the patient’s satisfaction perspective. It is dominated by the practice of triage or sorting patients based on their severity of illness or tolerance for waiting for treatment. The goal is to get the patient in front of the physician as soon as possible. This is achieved by uncoupling the triage and registration processes and ensuring that the triage has an appropriate capacity (physicians, nurses, beds) for every hour of the day, relative to demand.
- Doctor to Disposition Interval
Reduce bottlenecks by evenly distributing clinicians and resources. This deals with the in-emergency department segment of the patient throughput. The ED can be thought of as simply a collection of three servers the patients must navigate–doctors, nurses, and beds. The most commonly perceived problem of most EDs is a lack of beds. The need for beds can be reduced by keeping vertical patients vertical, implementing virtual beds in a result waiting area and optimizing laboratory and radiology turnaround times.
- The Disposition to Departure Interval
The final interval in the ED is the disposition to departure interval and is one of the most difficult to improve because it involves fixing hospital-wide flows. Emergency departments are often the last department to get a bed assignment.
In order to reduce flow time through any individual queue, ED departments must do one of the following:
Reduce average rate of patient arrivals into an ED queue
Reduce variation in the time between arrivals of patients
Reduce average physician and nurse service times
Reduce variation in service times
Add physician, nurse or bed server capacity or change the timing of server capacity.